Articular cartilage damage in the knee due to overuse or injury can be a difficult challenge for patients and providers to manage. Cartilage is a highly organized tissue with significant durability and poor intrinsic healing capacity. Trauma or degeneration can result in significant joint pain and functional impairment, and eventually lead to osteoarthritis – a debilitating condition.
 Figure 1: MRI showing a full thickness cartilage defect of the lateral femoral condyle
Figure 1: MRI showing a full thickness cartilage defect of the lateral femoral condyle
Early identification and treatment of cartilage damage can help to reduce pain, improve function, and delay the need for more definitive surgical options, such as knee replacement. At the Mercy Cartilage Repair and Joint Preservation Center, our highly trained specialists will work with you to determine the best treatment options, whether it be conservative treatment with physical therapy, injections, Orthobiologics, or surgical options.
 Figure 2: Arthroscopic image of a lateral femoral condyle cartilage defect
Figure 2: Arthroscopic image of a lateral femoral condyle cartilage defect
There are many treatment options that exist for managing focal chondral defects within the knee, including rehabilitation, cartilage transplant, and osteotomies, that depend on the size, location, and other important factors – such as patient age, activity level, alignment of the lower extremity and the presence of other injuries, such as a ligament or meniscus tear. Our providers are highly trained in the treatment of each of these factors and will help determine the best course of treatment to meet each patient’s individual needs.
Self-Management or Home Exercise Programs
Many of our patients are young and active individuals, and we advise them that it is important to maintain safe activities, such as walking and low impact exercises like a stationary bike, elliptical, or swimming. Living a healthy lifestyle and maintaining a healthy weight are important to aspects of managing cartilage damage in the knee.
Physical Therapy
Supervised exercise programs or formal physical therapy can be important to avoid the need for surgery, as well as both before and after a surgical intervention. We work closely with our physical therapists and have developed protocols to help patients maximize their outcome from whichever intervention we choose to pursue. Physical therapy is important to help maintain joint range of motion, correct gait impairments, strengthen the extremity after a period of protection, and to help guide our patients who hope to return to sport activities.
Unloader Bracing
Patients with isolated medial or lateral compartment cartilage damage with or without lower extremity malalignment may also benefit from unloader bracing. This is a specialized brace that will apply an external force to reduce the load in the damaged compartment of the knee, which can help with joint proprioception and reduce pain.
Anti-inflammatory Medications
Medications can also be a mainstay of treatment for managing knee pain due to cartilage damage. When patients are experiencing a “flare up” of joint pain, oral or topical anti-inflammatory medications can be helpful to get them through the acute phase. Over the counter medications, such as Ibuprofen or Naproxen can be helpful, as well as topical Diclofenac gel. Prescription strength medications such as Meloxicam can also be helpful for managing an acute episode of joint pain.
Intra-articular Injections
Corticosteroid injections – This is a strong anti-inflammatory medication that has been shown to be effective to reduce pain, and swelling, especially during an acute flare up. The benefits of steroid injections are relatively short-lived and typically last for about 4-6 weeks.
Hyaluronic Acid injections (Gel or Viscosupplementation injections) – Hyaluronic acid is a lubricant that all joints normally produce, and can be used to reduce inflammation and joint pain associated with cartilage damage. The data regarding hyaluronic acid injections is conflicting, though these can be effective in appropriately selected patients.
Platelet Rich Plasma (PRP) Injections – PRP is an Orthobiologic injection that is prepared from a patient’s own blood using a centrifuge to separate out the platelets from the red blood cells. PRP contains increased amounts of growth and differentiation factors that may be beneficial in the treatment of articular cartilage damage in the knee.
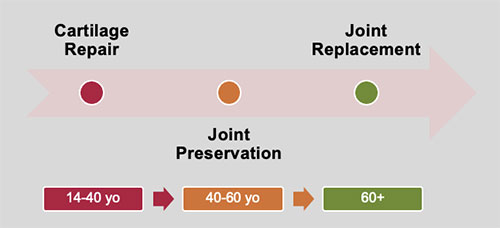
Please Note: These age ranges are general guidelines and helps to illustrate our goals of treatment, though each patient is treated with their best individual interests in mind
Cartilage Repair Surgical Options
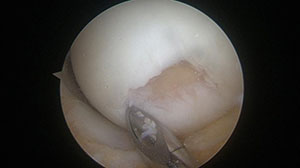 Figure 3: Arthroscopic image after debridement of cartilage defect
Figure 3: Arthroscopic image after debridement of cartilage defect
Marrow-stimulation techniques – For small focal chondral defects, marrow stimulation techniques such as abrasion arthroplasty, microfracture, or nano-fracture can be used to stimulate the subchondral bone to help cells and growth factors migrate to the area to form scar tissue or fibrocartilage. These techniques are typically performed with minimally invasive arthroscopic instruments and can be effective for small to medium sized defects. While this is not quite as durable as normal articular cartilage, this can be beneficial in certain instances.
Matrix Autologous Chondrocyte Implantation (MACI) – This is a surgical procedure for the treatment of full thickness cartilage defects in the knee. It is a two-stage surgical procedure, with the first stage being an arthroscopic procedure to assess the entire knee joint and the cartilage defect and perform a cartilage biopsy from a non-weight bearing area in the knee about the size of two tic-tacs if it is determined that the patient is a good candidate for MACI. The biopsy is sent to Vericel, a company based in Cambridge, Massachusetts where the cells can be stored frozen in liquid nitrogen for up to 2 years. After insurance approval for the second stage of treatment, and if the patient is continuing to have symptoms related to the cartilage defect, a surgical date is chosen. These cartilage cells are then cultured onto a collagen membrane and are shipped back to us.
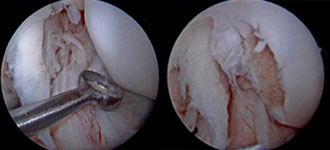 Figures 4 and 5: Arthroscopic image of taking a cartilage biopsy from the lateral femoral condyle
Figures 4 and 5: Arthroscopic image of taking a cartilage biopsy from the lateral femoral condyle
Implantation of the new cartilage cells is performed through an open surgical procedure where an approximately 6-10 cm incision is made in the front of the knee and the joint is opened with an arthrotomy. The cartilage defect(s) is then assessed and prepared by removing the damaged cartilage to create a stable rimmed defect and the MACI implant is then cut to precisely fit into your defect(s) and is glued into place. Once all of the defects have been addressed, the arthrotomy and incision are closed with dissolvable stitches. Patients will wake up from anesthesia with a large ACE wrap, a hinged knee brace and an ice machine wrapped around the knee. The procedure typically lasts 1-3 hours depending on the size and number of defects, as well if any concomitant procedures need to be performed such as an osteotomy. This is typically performed as an out-patient procedure, though some patients may be admitted to the hospital overnight to ensure their pain is adequately controlled and to start working with physical therapy the following morning.
The advantages of this technique are that it can be used to treat multiple defects within the knee that are of any size and shape and using a patient’s own autologous cartilage cells to grow new cartilage.
Osteoarticular Transfer System (OATS) – This surgical procedure involves the transfer of an autologous plug of cartilage and bone from a non-weight bearing area of the knee to a focal cartilage defect in the weight bearing surface. This technique can be used for defects smaller than 1 cm in size, and has the advantage of using a patient’s own bone and cartilage which has a superior healing potential versus allograft or donor tissue. The disadvantage of this technique is that we are removing bone and cartilage from one area of the knee, which can lead to abnormal stresses within the patellofemoral joint and pain at the donor site. Additionally, this technique is limited to only small defects that are about 1 cm in size or less.
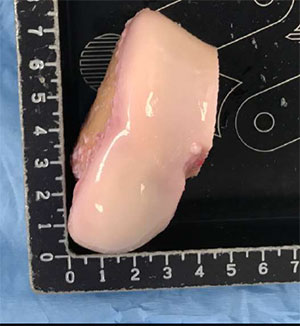 Figure 6: Osteochondral allograft of the distal femur condyle
Figure 6: Osteochondral allograft of the distal femur condyle
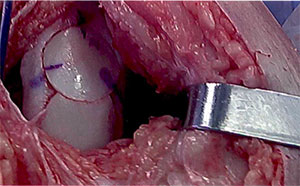 Figure 7: Osteochondral allograft two plug “snowman” technique
Figure 7: Osteochondral allograft two plug “snowman” technique
Osteochondral Allograft (OCA) – Osteochondral allograft transplant is a technique similar to the OATS procedure, but uses bone and cartilage transplant from an organ donor to replace the damaged cartilage in a patient’s knee. X-rays are used to match the size and shape of the patient’s knee to an appropriate donor. It can take as fast as two weeks or as long as six months to find an appropriate match for a patient. Tissue typing is not required as in other organ transplants with blood supply, such as kidney or heart. Rejection of bone and cartilage is exceedingly rare and typically occurs with persistent pain and swelling and failure of the allograft bone to incorporate at the recipient site in the knee. This procedure is performed through an open incision under general anesthesia. The knee joint is opened through an arthrotomy and the size and shape of the cartilage defect is identified and the appropriate size and shape is found on the donor graft to match the patient’s knee. The graft is then cut and gently press-fit into the defect in the knee to replace the damaged bone and cartilage. This can be performed as an out-patient procedure, though some patients may spend one night in the hospital to ensure adequate pain control and work with physical therapy the following morning. This surgical procedure has the advantages of replacing damaged cartilage with live chondrocytes in a mature matrix with underlying bone. This technique can be used for larger defects, or in the setting of a previously failed cartilage repair attempt that may have damaged the underlying subchondral bone. The disadvantages of this technique are the limited availability of grafts, high costs and risks of failure of the underlying bone can lead to large bone voids.
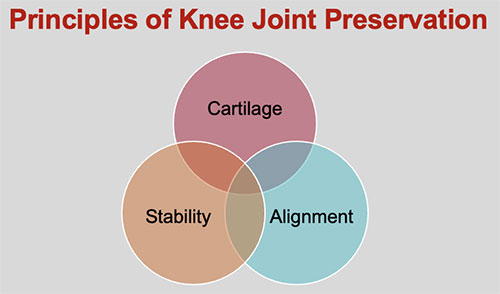
In order to have a successful cartilage repair treatment, these other factors must be addressed before or during the procedure to repair the damaged cartilage.
 Figure 8: Full length alignment x-rays with weight bearing axis drawn
Figure 8: Full length alignment x-rays with weight bearing axis drawn
Stability – Knee stability is often impacted from a ligament injury, such as an anterior cruciate ligament (ACL) tear. If a ligament injury is present or has led to cartilage damage in the knee, the ligament must be reconstructed or repaired before or during the cartilage repair procedure to ensure that the cartilage will be in the most favorable biomechanical environment for healing. Our providers have experience treating athletes at all levels with any combination of ligament injuries in the knee including the ACL, posterior cruciate ligament (PCL), medial collateral ligament (MCL), or posterolateral corner injuries including both primary and revision surgeries.
Alignment – Lower extremity alignment is measured with full length weight bearing X-rays to assess the amount of varus (bow-legged) or valgus (knock-kneed) in patients who are being considered for cartilage repair. A straight line from the center of the hip through the center of the ankle is used to illustrate the weight bearing line of the lower limb to determine if there is overloading in one compartment. If that is the case, then an osteotomy procedure must be performed in order to correct any malalignment to a neutral position in order to create a biomechanically favorable environment for optimal healing of a cartilage repair procedure or even to offload patients with more advanced arthritis who may not be candidates for a cartilage repair procedure.
 Figure 9: X-ray after High tibial osteotomy with plate and screws in place
Figure 9: X-ray after High tibial osteotomy with plate and screws in place
High Tibial Osteotomy (HTO)
This is a surgical procedure used to treat isolated medial compartment cartilage damage in patients who have varus malalignment (Bow-legged). HTO can be used as a treatment alone for patients with medial compartment arthritis who are too young to have a joint replacement or whose activity level is too high such that they could wear out an artificial joint prematurely. This can also be used in combination with a cartilage repair or cartilage transplant procedure to treat a focal area of damaged cartilage in the knee. The desired angle of correction is determined from pre-surgical x-rays and during surgery a cut is made partially through the tibia bone and a wedge of bone is added to correct the alignment to neural, and a special plate and screws designed to fit the tibia bone are placed to maintain the correction while the bone is healing. The advantage of this procedure is once the bone has healed, patients do not have any restrictions and may return to higher impact activities such as running or manual labor work. On average, these patients are aged 40-50, or younger if undergoing concomitant cartilage repair.
 Figure 10: X-ray after distal femur osteotomy with plate and screws in place
Figure 10: X-ray after distal femur osteotomy with plate and screws in place
Distal Femur Osteotomy (DFO)
This procedure is used to treat patients who have damage within the lateral compartment of the knee and have valgus malalignment (knock-kneed). In this procedure, the desired angle of correction is determined from pre-surgical x-rays and a cut is made in the femur bone and a small wedge of bone is placed to correct the alignment to about neutral and a specialized plate and screws are placed to maintain this correction while the bone is healing. This procedure may be used to treat isolated lateral compartment arthritis or in patients undergoing cartilage transplant procedures for the lateral compartment.
Tibial Tubercle Osteotomy (TTO)
This procedure is used to treat patients with patella (kneecap) maltracking with or without cartilage defects or patients with patellar dislocations or chronic instability. Often patients have had a previous patella dislocation that may have led to damage to the underlying cartilage and have developed chronic anterior knee pain or recurrent patellar instability. TTO may be performed in conjunction with a medial patellofemoral ligament reconstruction and/or cartilage repair procedures to the patella or trochlea.
OUR TEAM
Dr. Duerr serves as the Director of The Mercy Cartilage Repair and Joint Preservation Center. Dr. Duerr is recognized as an expert in performing lower extremity osteotomies and cartilage transplant and repair procedures and has been invited to lecture both nationally and internationally to teach other surgeons how to perform these techniques. He also has published several technique articles that he has helped pioneer while treating patients with these conditions. Dr. Duerr completed his training at Harvard University where he learned from Dr. Tom Minas and Dr. Andreas Gomoll – two of the world’s experts in cartilage repair and joint preservation. He then went on to join the faculty at The Ohio State University where he was an assistant professor in orthopedic surgery and sports medicine and was an integral member of the cartilage restoration program and taught numerous residents and fellows advanced techniques in joint preservation. In August of 2022, Dr. Duerr joined Mercy and hopes to bring his experience and expertise to treat patients in the St. Louis community who may be candidates for cartilage repair or joint preservation surgery.

